Treating Chondrosarcoma with Urgency and Compassion
Jeffrey T. Kramer,
President: Chondrosarcoma CS Foundation, Inc.
Introduction
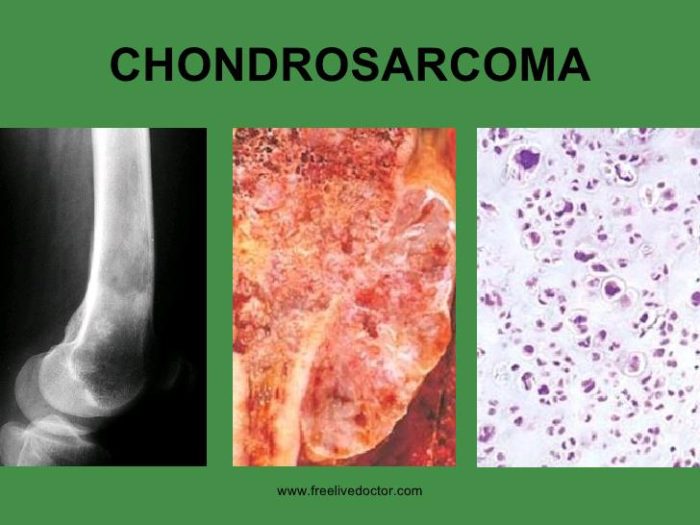
Cancer patients and their families perceive physicians and oncologists as experts in the treatment of cancer. We rely on them for the answers we seek and to prescribe the care that gives the greatest chance to beat cancer. With Chondrosarcoma that is not always the case. Chondrosarcoma is a rare bone and soft tissue cancer that has no established treatment protocol especially for high grade Conventional Chondrosarcoma and Dedifferentiated Chondrosarcoma. The only recommendation is surgical removal the tumor and that does not necessarily keep the cancer from returning or metastasizing.
Early diagnosis and detection of this cancer is also lacking. Many patients suffering from Chondrosarcoma are misdiagnosed and given misinformation. Months or even years go by before they are properly diagnosed. That missed valuable time allows this rare cancer to grow. With very little research and very few clinical trials that specifically address Chondrosarcoma, this makes the clinical management of the disease exceptionally challenging.
There are sarcoma experts but to our knowledge there are no known experts who specifically treat Chondrosarcoma. Chondrosarcoma is rare compared to other cancers effecting an average of 600 patients each year in the United States. Sadly, it has the same devastating effects as other cancers and should get the same levels of attention and study that many other forms of cancer receive.
Listed below is a case summary of Shayna Kramer who had advanced metastatic chondrosarcoma. The article is written by the patient’s father. Jeff Kramer is not a physician but is trained as a Basic Emergency Medical Technician and has a Master’s Degree in Clinical Psychology. He was with his daughter throughout the full course of her care and during that time, he reviewed the medical literature available in an effort to advocate and aide in the treatment and care of his daughter.
This article examines Shayna’s medical history, the problems that occurred and the implications on efforts to treat Chondrosarcoma with Urgency and Compassion. The intent of the paper is to give some direction to patients and families who have been newly diagnosed with Chondrosarcoma. It stresses the importance of advocating for patients’ treatment by (1) insisting to cast a wide net and examine all available treatment options and (2) verifying through second and third opinions that the treatment decisions made are the right decisions.
The article is also a message to the oncology community that there is a lot of work that needs to be done to find viable treatment options for Chondrosarcoma. Based on the case summary of Shayna Kramer changes also need to be made to offer compassionate and urgent care especially when Chondrosarcoma is rapidly spreading and in life threatening cases.
1. Summary of the Clinical History and Treatment
Shayna Elise Kramer from Bowie, Maryland was a 28-year old Female presenting with lower back pain with onset November 2015. An initial orthopedic examination evaluation, including an MRI, initially diagnosed her with scoliosis.
Increasing back pain and new neurologic defects were noted interfering with gait, prompting a CT scan which revealed a spinal mass. She was admitted to Johns Hopkins August 2016 and diagnosed with high grade (III) conventional chondrosarcoma involving the lumbar spine (L2/L3). The tumor was too large for resection-en-bloc, thus required two major surgeries. The first surgery- built rods to replace the L2/L3 spinal columns and the second surgery took the rest of the tumor from the spine and built a cage. Post-surgery, Shayna received thirty treatments of proton radiotherapy from the University of Maryland Proton Center. During her recovery from Proton Radiation and after 6 months of rehabilitation services Shayna was able to drive her car and work as a Teacher aide with Special Education preschoolers.
She remained in remission per the regional spinal MRIs she obtained every three months for the first year and six months on the second year post-operatively. Shayna also had an annual CT of her abdomen to screen for growth of a benign mass on her pancreas. The annual check on her pancreas incidentally suggested tumors on the lower visualized lung fields, but was later confirmed as fifteen bilateral metastatic tumors (average 2cm dia.). In addition, it was also discovered that Shayna had a metastatic tumor on her left great toe, which several doctors and oncology staff initially treated as an infection.
Shayna returned to Johns Hopkins for diagnosis and treatment. The biopsies of her lungs and great toe confirmed metastatic chondrosarcoma. In the absence of a nationally recommended treatment protocol, Shayna started off-study treatment with the multikinase inhibitor pazopanib (Votrient) 800mg per day. Initially it resulted in arrest of lung mass growth, however there was progression and new soft tissue masses involving multiple left MTP (toe) joints. Co-treatment of checkpoint-inhibitor immunotherapy began late July 2019 with pembrolizumab (Keytruda) every three weeks. However, it was later revealed from the literature that immunotherapy was not an effective treatment for Chondrosarcoma.
Shayna’s left great toe pain resulted in need for rapid advancement of narcotic regimen. There was nearly no precedent for chondrosarcoma distal joint metastasis, thus gamma radiation (15 sessions and half with heat treatments) was started and was ultimately effective for pain control. To help determine best treatment options, a genotyping study from Foundation medicine (FOUNDATIONONE®) identified potential susceptibility to radiation. She otherwise did not have typical biomarkers found in patients with conventional chondrosarcoma such as IDH1/2 nor other particular biomarkers. She was also found to have a borderline high tumor mutation burden of 19 (typically conventional chondrosarcoma has a very low mutation burden) suggesting potential responsiveness to immunotherapy or chemotherapy. Many biomarkers (both genetic and cell surface) required to determine chondrosarcoma trial eligibility however were not included in the Foundation medicine panel, and RNA gene expression panels were not available (at that time).
After the conclusion of the radiation to the left big toe, Shayna developed a high fever requiring Hospitalization in October 2019. A PET scan obtained during the hospitalization demonstrated diffuse progression and new lung/soft tissue and liver metastases, prompting plans to alter the regimen. In late October 2019, visual field defects and GI pain developed. Seven brain masses were identified, for which whole brain radiation was initiated along with corticosteroid therapy. Rapidly following initiation, severe abdominal pain developed, and was later diagnosed as colonic perforation requiring emergent open laparotomy where diffuse intraperitoneal metastatic disease and diffuse fecal contamination was identified. A hemicolectomy was performed and was treated with broad spectrum antibiotics. Surgeons, and internal and external oncologists had wide consensus to withhold treatment besides whole brain XRT until her abdominal wound healed. Her family wished Shayna to transition to home hospice care, with hopes that should her condition improve sufficiently to consider a therapeutic or palliative treatment.
Sirolimus and cyclophosphamide, used outside of a trial, were the initial planned options. Her poor functional status would not likely permit for significant delays of initiation nor another treatment option. As these had significant immunosuppression and adverse side-effect risks, alternatives for targeted treatment were pursued.
A trial was identified at Sloan Kettering Memorial of BA3021, an antibody drug (chemotherapeutic) conjugate for targeted treatment of solid tumors. Eligibility for the trial required ROR2 surface marker confirmation. In order to obtain surface marker staining, the IRB required in-person consent to participate in the study. She remained confined in her bed; and the family requested a waiver. After 2 weeks, the IRB convened and denied the waiver twice after a case was presented by doctors on the basis of compassionate care and to expedite evaluation. A social media blitz and a television investigative report initiated by Shayna’s father resulted in Sloan Kettering’s decision to change their position and obtain Shayna’s consent over the phone on November 12. Unfortunately, Shayna passed away two days later at home with family and friends. On November 22, 2019 the administrator at Sloan Kettering Memorial contacted Shayna’s father to indicate that she did have the ROR2 protein and could have been a candidate for the trial.
2. Implications of Treatment
Shayna had a recurrence of chondrosarcoma in her lungs and according to the medical literature the main metastatic site for chondrosarcoma, are the lungs. Many mistakes were made in Shayna’s care and treatment. From the care she received there was no established treatment protocol for Chondrosarcoma. Perhaps because Chondrosarcoma is a rare type of cancer and in research studies the disease gets lumped into trails with other sarcomas. Mistakes, errors, false assumptions and miscommunications occurred during the course of Shayna’s Care.
Misdiagnosis and Misinformation
When it comes to Chondrosarcoma Shayna’s disease progression defied many expert opinions, knowledge and expectations.
Early detection is lacking and is needed in diagnosing chondrosarcoma and there is a lack of information available about the disease. In November, 2015 Shayna was misdiagnosed with scoliosis and nine months elapsed before she was properly diagnosed. She was prescribed physical therapy and exercises which were ineffective in reducing her pain. The tumor grew to the size of a football causing Shayna to constantly loose her balance and fall. Then before surgery she had a foot drop and was confined to a wheel chair.
Other false assumptions and misinformation were communicated to the family. Post-surgery and prior to proton radiation the family was told that if the disease would reappear, it would be in the spine, when in fact it surfaced in her lungs and left big toe. The recurrence rate of high-grade chondrosarcoma is in fact high, and although local recurrence is most common, initial metastatic presentation in the lungs is routine. Oncology staff and doctors initially misdiagnosed the mass in Shayna’s left big toe as an infection given the rarity of appendicular metastasis.
In August 2018; Shayna started experiencing migraine headaches accompanied with auras which increased in frequency with the progression of her disease. An initial MRI on her brain was done in September 2018 to rule out any brain mass, and none were found at that time. Aggressive treatment of migraines was initiated with limited benefit. The family was told that chondrosarcoma does not affect the brain. Then in October 2019 a second MRI revealed that seven masses were found in her brain, raising concerns her headaches were due to malignancy. Metastatic chondrosarcoma to the brain had been described historically however, albeit very rare.
In late October 2019, when new visual field, headache and the chief complaint of abdominal pain symptoms developed, following identification of brain masses, no further abdominal evaluation was pursued. It was believed that the abdominal pain was due to the central nervous system findings, when in fact she had a developing colonic perforation. Family requests for abdominal imaging was declined, and it was recommended to provide gas tablets and antacids which were ultimately ineffective for the pain. Subsequent major abdominal surgeries, hemicolectomy and ileostomy, and subsequent bed confinement resulted.
The family was also told that the growth of conventional chondrosarcoma was slow, when in fact rapid growth occurred literally from head to toe occurring in the last five months of her life. The prognosis matched aggressive dedifferentiated chondrosarcoma far more closely than typical conventional chondrosarcoma. The delay of identification of the aggressive nature of her particular disease substantially altered any planning of other treatments and trials.
Mismanagement and Treating with Urgency and Compassion
There needs to be more compassion and urgency for cancer patients trying to obtain life-saving treatment and care. The priority of cancer research trials seems to be to obtain patients that qualify for a set of criteria and the trial itself appears to be very regimented as opposed to focusing on the individual patient’s needs. Medicine is designed to treat individual patients with compassion; clinical trials and research should do the same.
Shayna was not enrolled in any clinical trial. Clinical trials often require lengthy drug washout periods, and require tests/biopsies/procedures which may not otherwise be medically necessary or expedite care. Patients were required to not take medications for a minimum period of three weeks. They are also required to go through a litany of tests, biopsies and other procedures that pertain only to the study and not to the care of the patient, and patients have to travel to the institution to provide consent, provide samples and receive care in person.
In October, 2019 after discovering that immunotherapy was ineffective and that Shayna’s cancer had progressed rapidly in her lungs and other vital organs, it was decided to cease treatment. A trail at Johns Hopkins was recommended for Shayna but it took way too long to initiate the study and Shayna’s masses continued to grow at a rapid rate. She had no medication for over three weeks and her family was anxious to get Shayna on therapeutic/palliative medication. It was decided that sirolimus and cyclophosphamide would be prescribed. However, neurologic complications discovered in October prevented Shayna from ever starting that treatment. In several circumstances during the course of Shayna’s care it appeared that hurdles like getting insurance coverage and obtaining permissions moved at a snail’s pace. There was no urgency to get Shayna the care she needed despite the fact that her disease was rapidly progressing.
Better surveillance algorithms are needed, particularly including full body imaging, and especially with regards to periods of remission, and to screen for usual and unusual sites of metastasis. More comprehensive whole-body imaging, with a regular frequency, perhaps could have identified Shayna’s problems sooner.
Despite rapid tumor growth and progression of the disease on pembrolizumab (Keytruda) and
pazopanib (Votrient) a wide search was initiated in October 2019. A comprehensive search and eligibility
review for study treatment options should have been initiated at the outset of her diagnosis of
metastasis, given the obstacles getting appropriate staining and studies. By the time this was done
in October it was too late.
Shayna’s family helped identify the large majority of trial options for review, including the Sloan Kettering trial of BA3021 and numerous others. Shayna’s uncle directly contacted Sloan Kettering and identified that particular trial. It was difficult to identify trials which were not specific for Chondrosarcoma using search tools such as clinicaltrials.gov; many trials permitted other sarcomas or solid tumors. Although the Foundation report helped identify studies associated with a particular genotype, it did not identify multiple biomarkers and thus studies not part of the screening panel. A clearinghouse of all recruiting chondrosarcoma trials would have been helpful to more rapidly identify options based on markers, severity of disease, and other factors.
Biomarker staining/genotyping procedures should be done routinely and expeditiously for all patients with chondrosarcoma, not on-demand and one-by-one through siloed clinical trials. Rapid genotyping/phenotyping of a cancer with surface markers, genotypes and gene expression profiling could instantly identify a panorama of eligible drugs and trials; however, a comprehensive panel is not commercially available, FDA approved, nor routinely covered by insurance. The costs of some biomarker stains are negligible (such as immunohistochemistry) but restricted by proprietary antibodies and lack of certification for clinical use. Additionally, at least two institutions reported being unable to stain without study eligibility concerns due to IRB restrictions. This essentially prevented off-label and off-study compassionate use consideration of drugs.
A staining procedure was needed to determine if Shayna’s cells contained the ROR2 protein for the Sloan Kettering clinical trial. Although the staining procedure is simple and relatively inexpensive Sloan Kettering required that Shayna show up in person at the Center to give her consent to participate in the study. This was despite complications which prevented her from traveling. More compassion on the part of institutions of care are needed. Staining procedures should be done on demand and with faster turn-around time. It should be the standard to facilitate care as opposed to putting up barriers and road blocks to receive care. Whether it is a clinical trial or treatment the standard should be patient focused, compassionate and in some circumstances urgent care delivered to save or extend lives.

3. Implications to Improve Care and Treatment.
There is a lot to learn and discover about chondrosarcoma. That became obvious when we were told that Shayna’s disease did not behave like conventional chondrosarcoma; that it appeared in the lungs, spread rapidly throughout her body including in her brain. It was also obvious that no protocol existed to treat chondrosarcoma. Research and clinical trials are needed specifically to address chondrosarcoma to learn more about its progression and determine the most viable course of care.
Early diagnosis and better detection are vital in the treatment of Chondrosarcoma and that would include full body scans to confirm detection of masses. A lot of precious time was lost due to misdiagnosing, and if it wasn’t for an annual routine scan of her pancreas, we might not have known about the masses in her lungs. A national expert recommendation defending routine use of whole-body scans, later supported by evidence-based recommendations, should help improve obtaining permissions and getting insurance coverage.
There is essentially no research on interventions to maintain remission. Most chondrosarcoma research is focused upon treatment of metastatic disease or surgical/radiotherapy approaches of initial presentation. Prevention of local recurrence or metastatic disease with prophylactic medication, as has been identified in other malignancies such as breast and prostate cancer, might have been efficacious.
The medical literature suggests that a medication to serve as a prophylactic after Shayna’s first two surgeries on her spine could have been effective in containing the onset of her metastatic cancer as opposed to doing nothing. Other than proton radiation, Shayna received no prophylactic medications and the family relied upon hope that the cancer would not return. Research funding specifically targeting maintenance of remission interventions is urgently needed.
To educate the medical profession and families suffering from this disease a central repository should be developed that provides the relevant research, clinical trials, general information, information on surgical procedures, radiation, chemotherapies, immunotherapies and medications specific to Chondrosarcoma.
There also needs to be a repository or a place to provide staining on demand and faster turn-arounds similar to the Foundation that explores and examines biomarkers. Two weeks to get the results of a stain is unacceptable and in Shayna’s case it found she qualified for the BA3201 trial at Sloan Kettering but it was too late.
Requirements for clinical trials need to be flexible and take account the patient’s conditions and their right to obtain treatment. Clinical trials need to take into account the individual patient’s needs and when needed act with urgency to move the patient forward into the process. That includes removing the requirement to have the patient show up to the institution in person to provide their consent especially if their situation does not warrant travel.
4. Summary and Conclusions
Shayna fought hard to beat chondrosarcoma. Shayna’s wish and work since her diagnosis was to educate the public about this deadly disease and advocate for patients who are suffering from it. Her father made a promise to her that he would carry out her mission.
It became apparent in Shayna’s case that significantly more basic science research and clinical trials are needed to address the care for patients with this disease. Metastatic chondrosarcoma remains incurable and without a consistently effective treatment or guidance of care. Shayna had the luxury of access to national expert opinion at major academic hospitals and strong family advocacy, however even with such advice there was incomplete understanding of the options and studies available and negotiating urgent care within the institutional system was challenging. We have concerns for those patients, families and medical providers at local/regional hospitals having even fewer resources and advocacy available.
Based on Shayna’s case summary we learned the following:
a. The unusual aggressiveness and atypical metastatic distribution suggests atypical phenotypes of conventional chondrosarcoma exists. Additional research is needed to define these unusual phenotypes.
b. No centralized clinical parameters exist for chondrosarcoma. As is utilized with many other cancers, a serially updated expert consensus document/practice parameter is urgently needed. Presently, intermittent review articles are used to substitute for a centralized clinical parameter set. No review article to date has been comprehensive for diagnosis, phenotyping and treatment options.
c. As is common for rare diseases, no centralized national clearinghouse or registry for chondrosarcoma resources and information exist for patients and families.
d. An international patient registry (or sub-registry of an existing cancer registry) including genetic data, donated tissue, and clinical information can be utilized by researchers.
e. Research funding to study maintenance of remission is urgently needed, given a wide gap of the literature. This is a unique and likely the most effective time-frame to treat metastatic disease.
f. A specialized chondrosarcoma-specific genotyping/immunohistochemistry staining panel is required to efficiently and rapidly determine eligibility for research trial therapeutics. Most clinical trials for therapeutics require specific genotypes, cancer or immune system surface markers to determine potential for benefit. Most of these biomarkers are not available, even the most up-to-date commercial vendors (i.e. Foundation Medicine, Inc.). Custom panels are either not available, not reimbursable by insurers, nor CLIA-certified for clinical use. As such, medical researchers must presently be individually asked to assist with phenotyping out of goodwill, and may be restricted from doing so due to IRB criteria. These limitations all effectively prevent timely access to expanded (compassionate) use therapeutics. A better solution is necessary.
g. Treatment and care on all levels need to be compassionate, act with urgency and be patient specific. Requirements for clinical trials need to be more flexible and take account the patient’s conditions and their right to obtain treatment. That includes removing the requirement to have the patient show up to the institution in person provide their consent especially if their situation does not warrant travel.
To move forward and address the concerns and implications listed above, we created the Chondrosarcoma CS Foundation, Inc. The purpose of the Foundation is to educate the public about Chondrosarcoma and provide support and advocacy for patients and families that are suffering from this disease. Promote the improvement of treatment and care for these patients. We also advocate and promote positive changes including a viable treatment protocol, early detection, proper surveillance, more efficient and relevant information dedicated to Chondrosarcoma, and creating networking opportunities for sarcoma experts to specifically address Chondrosarcoma. Most importantly, we advocate for more compassionate care, cutting through red-tape and promoting the patient’s right to receive treatment especially if it is potentially life-saving.
In the long term, we seek the support of Cancer-related Medical Institutions and Organizations for guidance and assistance in our efforts to reach these goals. This includes fundraising support for research, and clinical trials specific to Chondrosarcoma to develop treatment guidelines, development of a clearinghouse/registry, a biobank with a specific biomarker panel, and help to reform compassionate use access and support for trial drugs. We believe bolstering support and identifying the needs of Chondrosarcoma patients will be a first step to help coordinate a unified phenotyping panel to improve the care and ultimately create a cure for Chondrosarcoma patients.
Jeffrey T. Kramer, M.S.; President;
Jeffrey T. Kramer, M.S.; President; created the Chondrosarcoma Foundation to honor his daughter Shayna’s legacy. Shayna expressed a desire to educate the world about Chondrosarcoma so she could help other’s suffering from this rare deadly bone cancer. Shayna lost her battle in November, 2019 and Jeffrey promised her he would create the CS Foundation. Mr. Kramer combines his years of experience in health care education, with his experience in broadcasting to produce film and videos. In addition, for the past 24 years, Jeffrey has been a certified Emergency Medical Technician and a Volunteer Firefighter for the Prince George’s County Fire Department.
Since October, 2000; Mr. Kramer has operated his own multimedia production company called Kramer Communications. In December 2006, Mr. Kramer traveled to the Jordan to produce a short documentary on the Iraq War entitled: The Price for Paradise which premiered on August 18, 2008 won a 2009 Regional EMMY for Best Cultural Documentary. In addition to his experience in broadcasting, Mr. Kramer has been an association executive and provided advocacy and leadership on Capitol Hill. He is the founder and former Executive Director of the National Treatment Consortium (NTC) and provided leadership in addressing challenging issues of treatment for addictions and mental illness and is responsible for commemorating September as Treatment Works Month.